Scott Witte, Ok Alone’s Vice President of Sales for North America, attended the Home Care 100 conference in Marco Island, Florida at the end of January, where he gained a deeper understanding of the staffing crisis in homecare.
“One of the main topics was staff turnover,” Scott noted. “Industry leaders repeatedly mentioned rates as high as 50%, highlighting the urgent need for better safety solutions to protect staff and improve retention within the industry.” However, further research revealed the situation was even worse.
The healthcare industry has always struggled with high turnover rates, but few sectors are as severely impacted as hospice and homecare. While registered nurses (RNs) in hospitals saw a turnover rate of 18.4% in 2023, ¹ the situation in hospice care is far more dire. Hospice RNs faced a 25.53% ² turnover rate in 2023, while licensed practical nurses (LPNs) and certified nursing assistants (CNAs) experienced even higher rates—often exceeding 30%. In the homecare sector, turnover has reached a staggering 79.2%,³ creating severe staffing shortages and disrupting patient care.
“This high level of turnover puts immense pressure on remaining staff and directly impacts the quality of care for the most vulnerable patients,” Scott explained. “Hospice and homecare workers provide compassionate, specialized care under demanding conditions, yet they often struggle with limited support, emotional burnout, and unsafe working environments.”

The Scope of the Problem: Turnover Rates in Healthcare
Turnover rates in healthcare remain alarmingly high, affecting hospitals, long-term care facilities, and homecare settings alike. Over the past five years, the average hospital has turned over 106.6% of its workforce,⁴ meaning that, on average, a hospital has replaced its entire staff more than once within that period. While hospital turnover is concerning, long-term care facilities like nursing homes face even greater challenges.
According to the Long-Term Care Community Coalition (LTCCC), the average nursing home reported a nursing staff turnover rate of 53.3%, with registered nurse (RN) turnover at 51.9%⁵. These high rates are often driven by staffing shortages, leading to heavier workloads, increased stress, and burnout among employees. Patient Care Technicians (PCTs) and Certified Nursing Assistants (CNAs) continue to experience the highest turnover rates in healthcare, as they serve on the front lines, performing critical daily tasks such as assisting with mobility, personal hygiene, and monitoring vital signs.
Turnover is particularly severe in homecare, where professional caregivers experience the highest levels of attrition. The median turnover rate for professional caregivers increased from 77.1% in 2022 to 79.2% in 2023, according to the 2024 Activated Insights Benchmarking Report (formerly Home Care Pulse) and marks the highest turnover rate since 2018 when turnover peaked at 81.6%.⁶ The report also found that nearly four out of five caregivers leave their job within the first 100 days of employment,⁷ highlighting the challenges of retaining workers in this field.

These figures underscore the systemic workforce instability in healthcare, particularly in long-term care and home-based settings. High turnover rates not only disrupt patient care but also place additional stress on remaining staff, creating a cycle that continues to worsen without intervention.
What Are the Main Factors Contributing to High Turnover Rates?
Several key factors contribute to persistently high turnover rates in healthcare, particularly in home health, hospice, and long-term care settings. Workforce demographics, job demands, and safety concerns all play significant roles.
1. Aging Workforce and Labor Shortages
Home health and personal care aides, along with nursing assistants, make up the majority of healthcare support jobs. These roles account for 71% of healthcare support positions, with 3.2 million home health and personal care aides and 1.4 million nursing assistants employed in the U.S. labor force. ⁹ As of May 2023, 931,000 home health aides and personal care aides were working specifically in home healthcare services. ¹º
Despite a steady increase in workforce numbers since 2021, the field faces challenges due to an aging workforce. Hospice and home health nurses have the highest percentage of individuals 60 or older, with many in the 40-plus range, compared to the average 25–39 age range in intensive and critical care settings.¹¹ Anticipated retirements will worsen existing labor shortages, driving further turnover.
2. Physical and Emotional Demands
Home health and hospice roles require intensive, direct care for vulnerable patients, leading to high levels of stress and burnout. Responsibilities range from assisting with daily activities and mobility to providing end-of-life support, all of which contribute to physical fatigue and emotional strain. The demanding nature of these jobs makes retention difficult, as many workers experience exhaustion over time.
3. Safety Concerns
Workplace safety remains a critical issue in healthcare, with violence and occupational injuries on the rise. Between 2019 and 2023, there were 481 fatal occupational injuries among healthcare practitioners, support staff, and technical occupations.¹² In Q2 of 2022 alone, more than two nursing personnel were assaulted every hour—amounting to 57 assaults per day and over 5,200 per quarter.¹³
The Bureau of Labor Statistics reports that healthcare continues to be the most injury-prone industry, with a 40% increase in injury and illness cases in 2020, reaching 806,200 incidents.¹⁴ Workplace safety is a major concern, with 54% of healthcare workers saying they would consider quitting if they experienced a violent incident.¹⁵ Persistent staff shortages further amplify safety risks, creating a cycle of attrition and vulnerability.
Healthcare workers have identified key measures that would improve their sense of safety, including:
- Panic button technology (55%)
- Safety procedure training (51%)
- Emergency alert systems (48%)
- A safety app with resources, plans, and emergency contacts (44%)¹⁶
With 90% of healthcare workers reporting violence from patients or caregivers in a single month ¹⁷, it is not surprising that many are considering leaving the profession. Addressing safety concerns is crucial in reducing turnover and improving retention in the healthcare sector.

What can be done to improve staff experiences?
Rather surprisingly, the easiest of the three major challenges in home healthcare to address— aging workforce and labor shortages, physical and emotional job demands, and safety concerns—is safety concerns. Effective solutions, such as employee safety monitoring apps, panic buttons, and emergency alert systems, are readily available and can be quickly implemented for immediate protection.
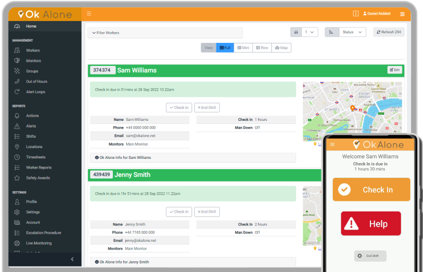
Workplace violence is a well-documented risk in home healthcare, and safety monitoring apps provide a vital layer of protection. These apps allow workers to check in regularly, ensuring employers and supervisors know their status and location. In emergencies, features like panic buttons, emergency alerts, and GPS locations enable rapid response times. Some apps include automated check-ins and worker-down detection, ensuring help is dispatched even if the worker is unable to call for it.
Scott noted that AI was a top priority and a major buzz at the Home Care 100 conference, with industry leaders emphasizing the need for automation and real-time integration. “With so much manual record-keeping and disconnected software systems, homecare organizations are looking for ways to streamline operations and improve efficiency—while still keeping their staff safe,”
A major advantage of employee safety monitoring apps is their accessibility—they can be downloaded directly to a smartphone, eliminating the need for additional devices. Using a safety monitoring app with API integration allows organizations to seamlessly connect with existing systems, such as their workforce management platforms, reducing the number of apps workers must use. By integrating safety features into tools that staff already use, companies can streamline operations, improve efficiency, and enhance user adoption.
This approach helps prevent app fatigue, where employees become overwhelmed by switching between multiple applications. Instead, with a single, consolidated platform, workers can access safety features, scheduling, reporting, and communication tools all in one place. By leveraging existing infrastructure through API integration, organizations can enhance staff safety without disrupting workflows or requiring additional training—ensuring a smarter, more efficient way to protect lone workers.
Conclusion
High turnover rates in homecare nurses remains a critical issue, with many staff leaving due to the dangerous nature of the role. Workplace violence, medical emergencies, and working alone in unpredictable environments contribute to stress, burnout, and safety concerns, driving staff away from the profession. Implementing an employee safety monitoring solution can help mitigate these risks, boost worker confidence, and improve retention.
Choosing a safety app with API integration allows organizations to seamlessly connect it with existing workforce management platforms, reducing the need for multiple apps. This streamlines operations, enhances efficiency, and improves user adoption, ensuring staff can access safety features without disrupting their workflow.
Scott emphasized, “By prioritizing staff safety with the right technology, homecare agencies can create a more secure, supportive, and sustainable work environment—ultimately reducing turnover and improving care quality.”
Beyond emergency response, safety apps help create a culture of preparedness, with built-in safety protocols, training resources, and incident reporting tools. By integrating these solutions, homecare agencies can improve worker confidence, reduce turnover, and ultimately enhance the overall safety of their staff.
References
2 – hospicenews.com
5 – IntelyCare: How to Reduce Nurse Turnover at Your Facility, 2024
6 – https://www.hcaoa.org/newsletters/home-care-turnover-rate-jumps-to-80hcaoa-is-here-to-help-members
7 – https://www.hcaoa.org/newsletters/home-care-turnover-rate-jumps-to-80hcaoa-is-here-to-help-members
9 – https://www.bls.gov/opub/ted/2021/healthcare-support-occupations-had-employment-of-6-4-million-in-may-2020.htm
10 – https://www.statista.com/statistics/185751/number-of-home-health-aides-in-the-us-since-2001/
11 – https://hospicenews.com/2024/05/28/the-state-of-the-hospice-nursing-workforce/
12 – https://www.bls.gov/news.release/cfoi.t03.htm
14 – https://www.osha.gov/healthcare
17 – https://www.performancehealthus.com/blog/hospital-incident-reporting-software-reduces-workplace-violence-in-healthcare 18 – https://www.performancehealthus.com/blog/hospital-incident-reporting-software-reduces-workplace-violence-in-healthcare

As an expert in lone worker content management, I possess an extensive knowledge base and experience in the area of lone working and safety monitoring. My expertise in this field encompasses a wide range of areas, including risk assessment, training, communication, and technology. I have a deep understanding of the unique risks associated with lone workers and have researched and written many projects and articles to educate people in how to mitigate these risks.
Throughout my time with Ok Alone, I have kept up to date with technological developments, legislative changes and regulations that have been introduced to help organizations ensure the safety of their lone workers.

